Your doctor has requested an endoscopic procedure for you. We will educate you about the procedure and all practicalities in the text below.
It is absolutely necessary to bring a companion / driver with you to your endoscopy appointment. Your physician will explain the results of the procedure afterwards, but your judgement will probably be impaired because of the sedation. By law, you are prohibited to drive after sedation and hospital regulations will not allow you to leave the hospital unaccompanied after sedation

Requested endoscopic procedure
Your doctor has requested an endoscopic procedure for you. You have been explained what this procedure entails and possible complications that may arise. You have also been asked whether you are taking any form of anticoagulants (blood thinners), aspirin or clopidogrel. You have been instructed to continue, discontinue or temporarily replace those medications. Please contact your doctor if you have questions about the instructions.
What preparation is required?
- You will have to bring a companion / driver. Please organize this prior to the procedure
- You will receive specific instructions for the bowel prep in a separate flyer
- For procedures in the morning hours, you will have to start fasting from midnight onwards. You have to finish drinking the bowel prep two hours before the procedure starts. If the procedure takes place in the afternoon, it is allowed to have a “small breakfast” before 8 o’clock in morning (please check the dietary instructions in the bowel-prep flyer). You are permitted to take your medication with some water. Fasting means: do not drink, eat or smoke.
Appointment
You will receive your appointment from the Endoscopy front desk. If the appointment doesn’t suit you, please call 043-3877700.
Your doctor will prescribe the type of bowel preparation that is best for you. You have also received the recipe. If not, please contact your doctor. You will receive a separate flyer from the Endoscopy front desk with the specific instructions on how to use the bowel prep.
Your companion/driver
You are required to bring a companion/driver. Please organize this prior to the procedure. Your companion will wait in the waiting room during the procedure and will escort you home. There are no visitors allowed in the endoscopy suite during the procedure. If you do not bring someone with you, the procedure will not take place.
Conscious sedation
When your doctor requested the endoscopic procedure, the decision is made that you will undergo the procedure under conscious sedation. We use a combination of a hypnotic drug (midazolam) and a painkiller (fentanyl) to make you comfortable. This is not general anesthesia! We do not promise you falling asleep or feeling or hearing nothing at all during the procedure. We expect to perform the procedure without problems, with you being comfortable; most people do not remember anything or very little after the procedure.
Because people tend to breathe more superficial, we will connect you to a monitor to cover your heartbeat, blood pressure and saturation.
By law, you are prohibited to engage in traffic or make important decisions (like signing a notarial deed) after receiving conscious sedation. You are strongly advised not to drink alcohol after the procedure.
Day of the procedure
You will reach the Endoscopy department in the MUMC+ via walking route “G2 groen”. Please sign in at the front desk. You are kindly requested to arrive 30 minutes before the appointed time.
In the endoscopy suite, we double-check your name and date of birth. Hereafter we will put a band around your wrist with this information on it.
We ask you to take off your coat and to undress your lower body in the changing room (you may keep on your socks). After undressing you may cover yourself with a sheet (provided by us) and sit down on the bed in the endoscopy suite. We will insert an iv needle (to be used for the sedation) and connect you to the monitor.
We will do a “time out procedure” to check your name and date of birth again. We will also check if we have anticipated the correct endoscopy procedure, what blood thinning medication you use or have discontinued/replaced, allergies for medications, pacemakers or hip or knee replacements. This is also the best time to ask questions to us.
After the time out, the procedure will start.
- We ask you to bring your own (shopping) bag. We will store your clothes in it during the examination.
- If you want/need to take your medication after the examination, please bring it from home. We do not stock them.
- You will receive a sandwich and coffee/tea in the recovery room. If you have any allergies or food intolerances, please bring your own sandwich.
Upper endoscopy / gastroscopy
Upper endoscopy lets your doctor examine the lining of the upper part of you gastrointestinal tract, which includes the esophagus, stomach and duodenum (first part of the small intestine). Your doctor will use a thin, flexible tube called endoscope, which has its own lens and light source, and will view the images on a video monitor. You might hear your doctor or other medical staff refer to upper endoscopy as gastroscopy of esophagogastroduodenoscopy.
Before starting the procedure, you will usually get a very small drink with anti-foam medication. This allows for better vision of the lining of the stomach. If you have dentures, we ask you to take them off. Also, some local anesthetic is sprayed in your throat. After all this, the nurse places a plastic ring between your jaws (this protects you teeth and our endoscope).
You’ll then lie on your left side as the doctor passes the endoscope through your mouth and into the esophagus, stomach and duodenum. The endoscope doesn’t interfere with your breathing. Most patients consider this procedure only slightly uncomfortable.
Possible complications (gastroscopy)
Although complications can occur, they are rare when doctors who are specially trained and experienced in this procedure perform the examination. Bleeding can occur at a biopsy site or where a polyp was removed, but it’s usually minimal and self-limiting.
When there is food retention in the stomach, this might be burped up and enter the airway causing a respiratory infection. Also, after forceful burping or difficult passage of the endoscope, the lining of esophagus or stomach may bleed. Your throat may be a little sore for a day. A very rare complication is a tear in the esophagus (e.g. when there are strictures in the esophagus).
Although complications after upper endoscopy are extremely rare, it’s important to recognize early signs of possible complications. Contact your doctor immediately if you have a fever after the examination or if you notice trouble swallowing or increasing throat, chest or abdominal pain, or bleeding, including black stools. Note that bleeding can occur several days after the procedure. You will receive a note when leaving the endoscopy suite with the numbers you have to call in case of problems following the endoscopy.
after the upper endoscopy, we will do the colonoscopy
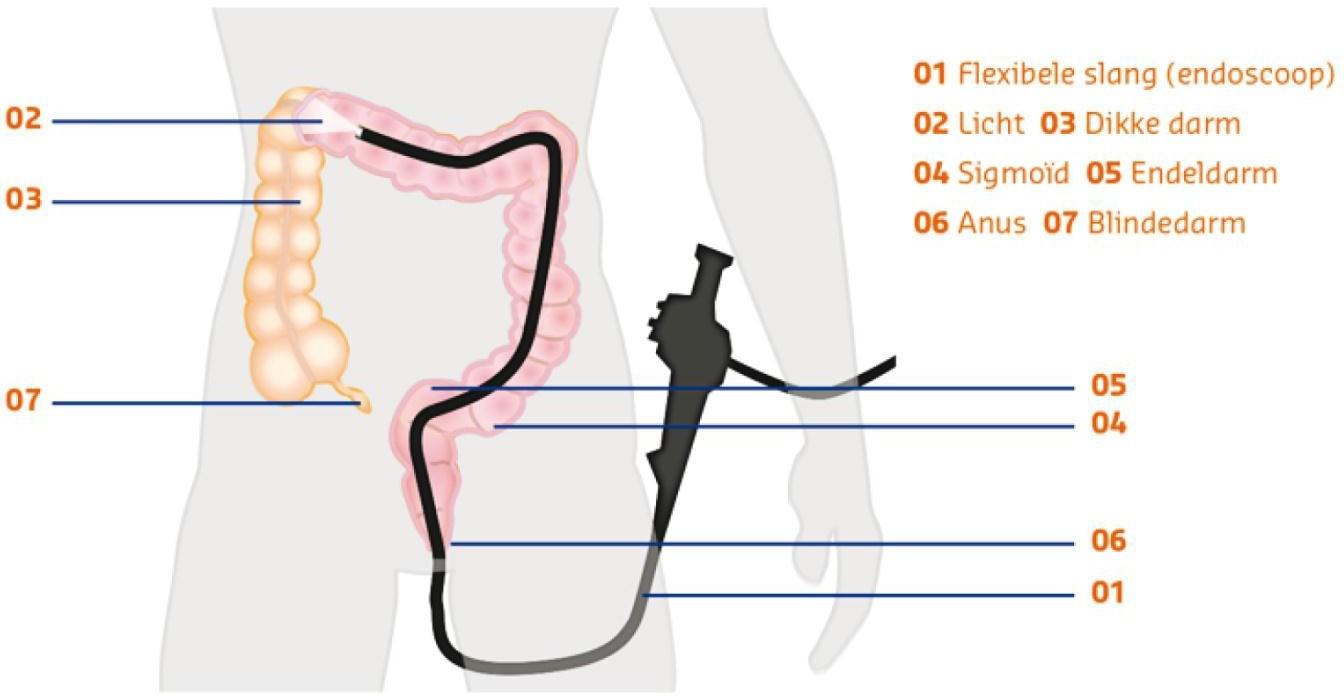
Colonoscopy
Colonoscopy enables your doctor to examine the lining of your colon (large intestine) for abnormalities by inserting a flexible tube as thick as a finger into your anus and slowly advancing it into the rectum and colon. You will lie on your left side while the physician advances the colonoscope through your colon (and possibly the last part of the small intestine). The doctor will examine the lining carefully as she or he slowly withdraws the colonoscope. The procedure itself usually takes 15 to 30 minutes.
Colonoscopy is well-tolerated and rarely causes much pain. You might feel pressure, bloating or cramping during the procedure. Sometimes the doctor will ask you to turn to your back or right side during the procedure in order to pass the endoscope easier through the colon and make you more comfortable. At times, a nurse will support your abdomen from the outside to prevent looping of the endoscope.
In some cases, the doctor cannot pass the colonoscope through the entire colon to where it meets the small intestine. Sometimes it is necessary to do another procedure or scan instead. Your doctor will tell you and your companion about this directly after the procedure.
Possible complications (colonoscopy)
Colonoscopy/sigmoidoscopy and polypectomy are generally safe when performed by doctors who have been specially trained and are experienced in these procedures.
One possible complication is a perforation, or tear, through the bowel wall that could require surgery. Bleeding might occur at the site of biopsy or polypectomy, but it’s usually minor and self-limiting. Some patients might have a reaction to the sedatives or complications from heart or lung disease.
A different form of complication is a “missed leasion”. When a polyp is located just behind a fold or when the bowel is not completely clean, we might miss something.
Although complications after colonoscopy are uncommon, it’s important to recognize early signs of possible complications. Contact the Endoscopy front desk if you notice severe abdominal pains, fever and chills or rectal bleeding of more than a few drops. Note that bleeding can occur several days after the procedure. You will receive a note when leaving the endoscopy suite with the numbers you have to call in case of problems following the endoscopy.
Taking biopsies or removing tissue/polyps
If your doctor thinks an area needs further evaluation, he or she might pass an instrument through the endoscope to obtain a biopsy (a sample of the lining) to be analyzed. This will usually not cause any pain, but may lead to some blood loss. If the doctor finds polyps during the examination, they can usually be removed in the same procedure. This is done by cutting them loose with a wire loop or using a technique called “snare polypectomy”. That technique involves passing a wire loop through the endoscope and removing the polyp by using an electrical current. You should not feel pain during the polypectomy.
Teaching hospital
The Maastricht University Medical Center is a teaching hospital. It may be possible that the endoscopic procedure is performed by a trainee under supervision of a certified gastro-enterologist. At times, medical students are present to watch; your permission will then be specifically asked.
Immediately after the procedure
After the procedure you will stay in the recovery suite for 1 hour or so. When you are fully awake, we will provide you with something to drink and eat.
On leaving the endoscopy suite, you will receive a note with a telephone number to call when you might experience a complication after the procedure. Furthermore, the card provides you with some guiding rules, follow up appointments and (when applicable) advice on your blood thinning medication.
Results of the procedure and further treatment
On leaving the endoscopy suite, you will receive a note reminding you of your appointment for the results of the procedure and further treatment.
Contact
If you have any questions about the procedure after reading this flyer, please contact your doctor. If you have questions about practicalities, please call the Endoscopy front desk: 043-3877700 (workdays between 8.00 AM and 4.30 PM) or send an email to endoscopie@mumc.nl (blank)
The Maastricht UMC+ endoscopy department has taken great care in compiling this folder. Nevertheless, it is possible that the published information is incomplete or incorrect. However, the MUMC+ does not accept any liability for this. The MUMC+ also excludes liability for damage resulting from or related to the use of the information published in this folder/on this website.
